Select a button to be taken to that section to learn more
Surgery: laparotomy versus laparoscopic/robotic
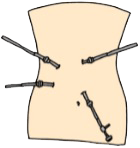
Laparoscopy
Most surgeries for Crohn’s disease, ulcerative colitis or colorectal cancer can be performed laparoscopically or with the robot. This allows the surgeon to make a few small incisions through which the laparoscopic instruments are introduced, allowing the surgeon to operate on the bowel. Laparoscopic or robotic surgeries are associated with faster recovery, reduced postoperative pain, decreased risk for wound infection and lower risk for incisional hernias. Other possible benefits include better cosmetic result, reduced risk for bowel obstruction and improved preservation of fertility, especially in women.
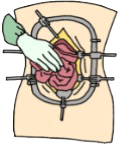
Laparotomy
However, when laparoscopic or robotic surgery is not possible, open surgery (laparotomy) is indicated and usually happens through an incision on the midline. The surgeon will try to minimize the length of incision whenever possible.
Crohn’s Disease
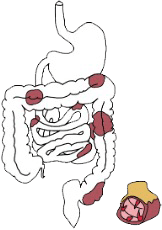
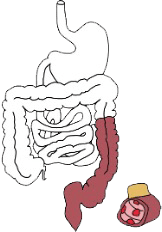
Crohn’s disease (CD) is a chronic inflammatory disease of the bowel, that can involve the complete gastrointestinal tract, resulting in a myriad of symptoms depending on the severity as well as the location of the disease. Patients with Crohn’s disease can develop diarrhea, abdominal pain, intestinal obstructions, along with many other symptoms, which may result in significant weight loss. Long standing inflammation of a bowel segment can lead to either strictures or fistulas of that segment . Fistulas are abnormal connections between the organs (e.g., the intestine, bladder and the skin), and can lead to complications such as infection. One third of all patients with Crohn’s disease will also develop peri-anal Crohn’s disease, in many cases resulting in peri-anal fistulas. Patients are usually treated with several types of drugs to control the inflammation. However, some patients will require surgery during which the surgeon will deal with the diseased segment.
Surgery for Crohn’s Disease
Most patients develop Crohn’s disease in the last segment of their small bowel, which is called the terminal ileum and is connected to the colon through the ileocecal valve. An ileocolic resection for Crohn’s disease involves the removal of the terminal ileum. This procedure is commonly performed to manage complications of Crohn’s disease, such as strictures, fistulas, or severe inflammation. By removing the diseased sections, your surgeon aims to alleviate your symptoms (e.g. pain, cramps, bloating, diarrhea) and improve your quality of life.
While ileocolic resections can provide significant relief, it is not a cure for Crohn’s disease and may necessitate ongoing medical treatment to prevent recurrence and maintain remission. It is therefore important to remain in contact with your gastroenterologist, who will decide together with you about the best post-surgical strategy to minimize the chances of disease recurrence.
Other patients will develop Crohn’s disease more upstream in their small bowel. In those cases, surgery can be indicated as well, during which a small bowel resection will be performed. In majority of cases the bowel will be reconnected and a (temporary) stoma will not be required.
In some cases, although rare, a temporary stoma may be required, especially in patients who are very sick with significant weight loss or are on a higher dose of steroids. However, in most cases, the bowel is reconnected and a stoma is not required.
A strictureplasty is a surgical technique used to manage some types of strictures (narrowed sections) of the intestine in patients with Crohn’s disease. Unlike resections, strictureplasties preserve the bowel by widening the narrowed segment without removing it. This procedure can be particularly beneficial for patients with multiple strictures or those at risk of short bowel syndrome.
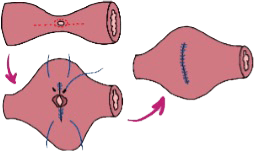 Strictureplasties aim to alleviate symptoms and improve intestinal function, often resulting in long-term relief for Crohn’s disease patients. It is often performed in combination with “resection” to minimize the length of bowel removed during surgery. There are different types of strictureplasties, according to the length of bowel involved.
Strictureplasties aim to alleviate symptoms and improve intestinal function, often resulting in long-term relief for Crohn’s disease patients. It is often performed in combination with “resection” to minimize the length of bowel removed during surgery. There are different types of strictureplasties, according to the length of bowel involved.
However, a strictureplasty is not always possible and your surgeon will make that judgement during surgery.
In Crohn’s disease, the colon, rectum and/or anus may be involved, and patients may require surgical removal of all or parts of these organs. Depending on the length and the number of the diseased segment, a short or long resection may be indicated.
In Crohn’s disease, the colon, rectum and/or anus may be involved, and patients may require surgical removal of all or parts of these organs. Depending on the length and the number of the diseased segment, a short or long resection may be indicated.
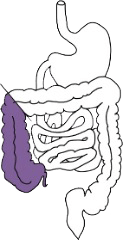
If the right part of the colon is diseased, a right hemicolectomy is possible, only removing the right half of the colon.
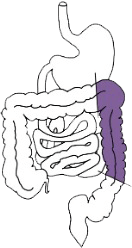
If the left part of the colon is involved, a left hemicolectomy is possible, preserving the right part of the colon and the rectum.
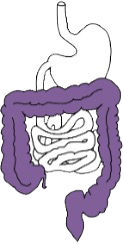
In case of extensive disease, a (sub)total colectomy is possible, removing the total colon while keeping the rectum and anus.

In case the rectum and anus are also involved, a proctocolectomy, the surgical removal of the colon, rectum and possibly the anus, is performed, usually resulting in a permanent stoma.
The large bowel (i.e., colon and rectum) begins at what is referred to as the ileocecal valve and runs to the anus. Its total length is approximately 1.5m long. The last 20cm of the large bowel is called the rectum and is situated just above the anus. The rectum functions as a reservoir to collect your stool, in turn regulating your bowel movements. Patients who had their rectum removed have a higher bowel frequency (i.e., you would be using the toilet more often). The anus refers to the opening at the end of the bowel through which the stool is expelled during a bowel movement. It is complex organ that mainly consists of muscles (the anal sphincter) to help preserve continence. It is perfectly possible to live without a rectum and no specific nutritional modification are required in anyone with a normally functioning small bowel.
A stoma refers to bowel coming through and out of the abdominal wall, to collect one’s stool in a plastic bag. A stoma is sometimes required in Crohn’s disease for reasons listed below:
- Patients with severe Crohn’s disease, in their colon or at their anus, may require a diverting stoma to allow the disease to be better controlled. By avoiding stool to be passed through the diseased segment, the symptoms of the disease will be reduced.
- Patients with anal Crohn’s disease may require a stoma to control the symptoms of fistulas, reducing the local infection and inflammation as well as decreasing the amount of drainage through the fistula
- Patients undergoing a proctocolectomy (i.e., removal of colon, rectum and anus), because of extensive disease, will have a permanent stoma to manage their bowel movements.
- Patients with bad terminal ileal (last part of small bowel) disease are also at risk for temporary stomas.
A stoma can be permanent or temporary, depending on the reason and the type of surgery performed. It can also be formed with your small bowel (ileostomy) or colon (colostomy). Your surgeon will be able to clarify which stoma is required for each individual case.
It is, however, important to understand that patients with a stoma report a very good quality of life in majority of cases, as it allows patients to resume a normal professional, social and physical life without restrictions.
Please refer to the following resources to better understand stomas and how to manage it:
- mountsinai.on.ca [MSH website for patients/families and professionals]
- ostomycanada.ca or 1-888-969-9698 [Ostomy Canada Society]
- ostomycanada.ca/support/canadian-chapters/ [Ostomy Canada Society: information regarding peer support groups]
- ostomytoronto.ca [Ostomy Toronto]
- crohnsandcolitis.ca [Crohn’s and Colitis Foundation of Canada]
- dietitians.ca/eatwell [Provides basic information on healthy nutrition; includes Canada’s Food Guide]
- coloplast.ca [Information on Coloplast ostomy products]
- hollister.ca/en-ca [Information on Hollister ostomy products]
- convatec.ca [Information on ConvaTec ostomy products]
- j-pouch.org [For individuals with the pelvic pouch or ileoanal reservoir]
- cancer.ca [Canadian Cancer Society]
- cancer.org [American Cancer Society]
Ulcerative Colitis
Ulcerative colitis is a chronic inflammation limited to the colon and rectum and is usually treated with medication. However, about 15% of all patients with ulcerative colitis will require surgery for multiple reasons. Some examples include the lack of response to medical treatment or the presence of (pre-)cancerous lesions (low- or high-grade dysplasia) in the colon. The surgery can require to be scheduled urgently in very sick patients or can be scheduled electively, meaning that you and the surgeon decide (elect) when the surgery happens. In most cases, the purpose of surgery is to remove the colon and rectum. The rectum is the last part of the colon and functions as a reservoir to collect the stool in order to allow the person to go to the toilet at regular times. However, in patients with ulcerative colitis, the rectum is inflamed and causes high bowel frequency and urgency. To replace the rectum, a J-pouch is formed out of a patient’s small bowel. This J-pouch refers to a reservoir in the shape of a J, and it does not require an implantation of any foreign body. Because patients in need of a J-pouch are often sick with active inflammation, the full surgical treatment is performed in stages which are a few months apart of each other.
Surgery for Ulcerative Colitis
In most cases, a subtotal colectomy will be performed as first stage. This procedure involves the removal of most of the colon, leaving the rectum in place. This surgery allows the patient to recover from symptomatic ulcerative colitis, while avoiding the need to reconnect the bowel as it could increase the risk of infection in a sick patient. It dramatically improves the symptoms and restores the patient’s quality of life. In fact, patients report to feel much healthier very soon after this surgery. Patients are left with a temporary ileostomy for a few months until bowel continuity (i.e., stoma closure) is restored.
Completion total proctectomy is performed in patients with a previous subtotal colectomy, who do not qualify for a J-pouch or want to keep their stoma. This could be due to patients having:
- a poor anal function not allowing to proceed with a J-pouch, or
- a (pre-)cancerous lesion not allowing to keep their anus.
This procedure involves the removal of the remaining rectal stump and the anus, which will result in a little scar at the level of the anus. Possible drawback of the surgery includes delayed healing of the anal wound, which in rare cases remains as an open wound with ongoing discharge. However, in most cases, the skin will heal, and a small scar will remain with excellent aesthetic result.
Pelvic Pouch
Ileal pouch-anal anastomosis (IPAA) is a surgical procedure, also known as pelvic pouch procedure, used in the treatment of inflammatory bowel disease (IBD), specifically ulcerative colitis and familial adenomatous polyposis. IPAA may also be possible in select cases of Crohn’s disease. During IPAA, the colon and rectum are removed in various stages, and a pouch is created from the end of the small intestine (ileum). This pouch is then connected to the anus, allowing for the passage of stool. IPAA aims to alleviate symptoms such as diarrhea and abdominal pain while preserving bowel continuity and avoiding the need for a permanent ostomy. It is often considered for patients who have not responded to medical therapy or who have complications such as dysplasia or refractory disease.
The large bowel (i.e., colon and rectum) begins at what is referred to as the ileocecal valve and runs to the anus. Its total length is approximately 1.5m long. The last 20cm of the large bowel is called the rectum and is situated just above the anus. The rectum functions as a reservoir to collect your stool, in turn regulating your bowel movements. Patients who had their rectum removed have a higher bowel frequency (i.e., you would be using the toilet more often). The anus refers to the opening at the end of the bowel through which the stool is expelled during a bowel movement. It is complex organ that mainly consists of muscles (the anal sphincter) to help preserve continence. It is perfectly possible to live without a rectum and no specific nutritional modification are required in anyone with a normally functioning small bowel.
The whole J-pouch procedure is performed in one single surgery. The colon and rectum are removed, and a J- pouch is formed during the same procedure. This is considered in very rare cases, which your surgeon will explain more in detail.
This is similar to the 1-stage approach, where the colon and rectum are both removed and the J-pouch is formed during the same surgery. However, the J-pouch is being diverted by an ileostomy to prevent any stool from passing through the pouch.
The second surgery happens about 6-12 weeks later to close the stoma. This will reconnect the bowel, allowing stool to pass normally through the anus again. This second surgery is a much smaller operation.
The modified 2-stage approach involves two surgeries, although slightly different from the 2-stage approach. The first surgery includes a subtotal colectomy, where only the colon is removed, leaving the rectum behind. A temporary ileostomy is also placed for about 3 – 6 months.
The second surgery is then performed to remove the rectum (completion proctectomy) and to make the J-pouch. However, no further ileostomy is placed, and the pouch will be functional straightaway.
The only difference of the 3-stage with the modified 2-stage is the fact that a stoma is placed at the end of the second surgery, requiring a third surgery to close the stoma after 6 – 12 weeks.
A patient with a stoma can expect a very well-preserved quality of life, allowing for normal daily activities without any major restrictions. Bowel frequency is reported to be between 5 and 8 bowel movements over 24 hours. However, bowel movement is usually not associated with any urgency, allowing patients to defer when needed.
Some patients will develop pouchitis which is an inflammation of the pouch. This will result in frequent bowel movements with urgency, although usually responding very quickly to antibiotics. A minority of patients develop chronic pouchitis requiring more prolonged treatment.
A fraction of patients (10 – 15%) will end up with pouch failure requiring a permanent ileostomy. This can occur for multiple reasons. However, a large majority of patients will keep their pouch for the rest of their lifetime.
Some patients may opt for a permanent stoma even when a pouch is possible. A permanent stoma is also a good option resulting in good quality of life. Don’t hesitate to discuss this with your surgeon.
Treatments for Colorectal Cancer
Some patients with Crohn’s disease will develop the so-called anal Crohn’s disease, mostly referring to peri- anal fistulas. A fistula is a connection between the inside of the anus (internal opening) and the skin around the anus (external opening). Peri-anal fistulas are very challenging to treat and require concurrent treatment by your gastroenterologist and surgeon. The role of the surgeon is to treat any abscess (cavity filled with pus) present, usually requiring surgical drainage in the operating room, and to minimize the risk for an abscess to. In selected cases, a surgical attempt to close the fistula can be attempted.
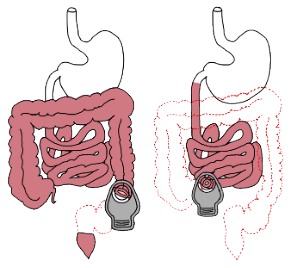
Rectal resection is a surgical procedure used to treat rectal cancer by removing the affected portion of the rectum. The types of rectal resection include Low Anterior Resection (LAR) and Abdominoperineal Resection (APR).
Low Anterior Resection (LAR) [insert graphics]
Abdominoperineal Resection (APR) [insert graphics]
Local excision with trans-anal access is a minimally invasive surgical technique used for early-stage colorectal cancer, particularly when tumors are small and confined to the rectal wall. This procedure involves removing the tumor and a margin of surrounding healthy tissue directly through the anus, using specialized instruments. It aims to preserve normal bowel function and avoid the need for more extensive surgery. Postoperative care focuses on managing pain, monitoring for complications such as bleeding and infection, and ensuring proper healing.
Bowel resection for colorectal cancer involves the surgical removal of the affected segment of the bowel, including adjacent healthy tissue and regional lymph nodes, to ensure comprehensive tumor excision and accurate staging. The procedure often includes a primary anastomosis, reconnecting the remaining bowel ends to preserve gastrointestinal continuity. This surgery can be performed via open or minimally invasive techniques, such as laparoscopy, which offer benefits like reduced postoperative pain and quicker recovery.
Treatment of Perianal Crohn’s Disease
In most cases, a subtotal colectomy will be performed as first stage. This procedure involves the removal of most of the colon, leaving the rectum in place. This surgery allows the patient to recover from symptomatic ulcerative colitis, while avoiding the need to reconnect the bowel as it could increase the risk of infection in a sick patient. It dramatically improves the symptoms and restores the patient’s quality of life. In fact, patients report to feel much healthier very soon after this surgery. Patients are left with a temporary ileostomy for a few months until bowel continuity (i.e., stoma closure) is restored.
In case of a simple, superficial fistula, a fistulotomy is a very successful procedure. An incision is made along the length of the fistula tract, opening it up and promoting healing from the inside out. When this procedure is indicated, the fistula is treated in majority of the cases. However, the downside is that some muscle is always transected, subsequently putting the patient at risk for incontinence. Therefore, your surgeon must consider this technique carefully to reduce the risk for fecal incontinence, especially in Crohn’s disease patients.
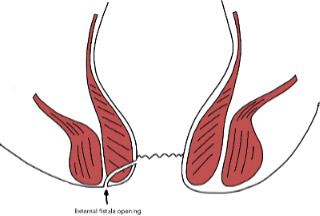
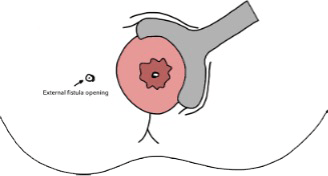
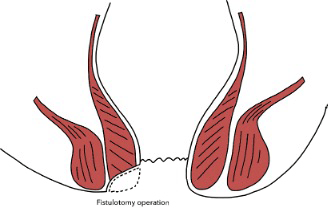
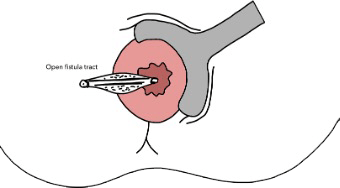
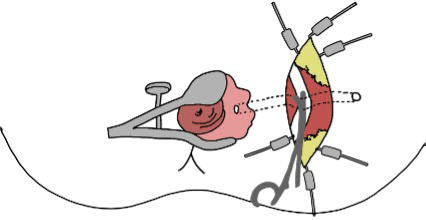
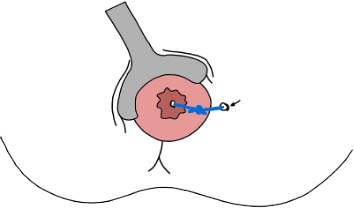
A seton is a small, looped rubber band. Placement of seton drains is a common surgical intervention for managing perianal Crohn’s disease and benign perianal diseases, aimed at keeping the fistula open and to avoid recurrent peri-anal abscesses. Your surgeon will discuss with you when the seton can be removed.

Surgical Options
There are 2 main surgical option to repair a fistula, through which your surgeon will try to close the opening in the anus (internal opening).
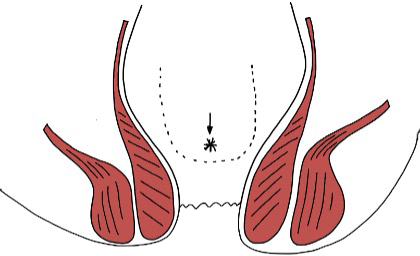
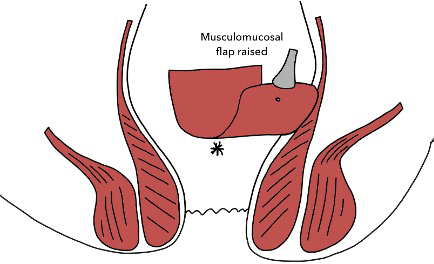
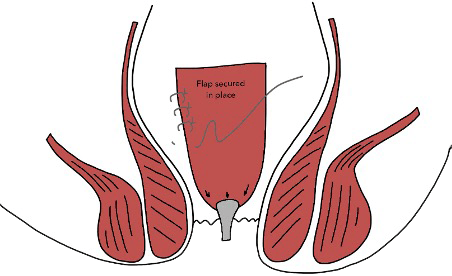
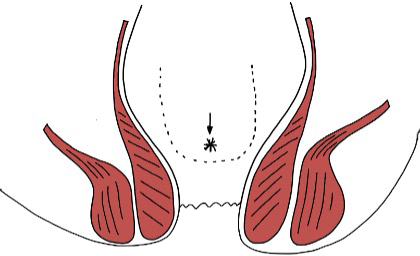
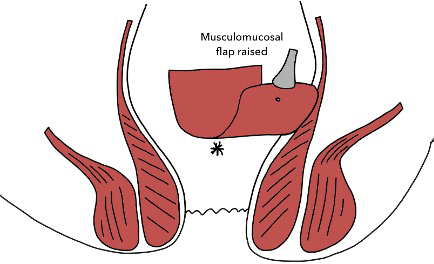
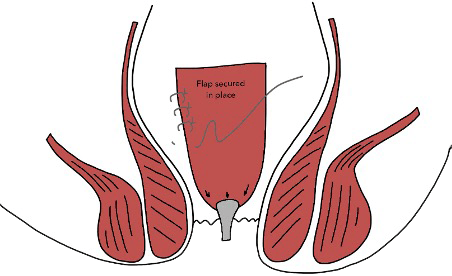
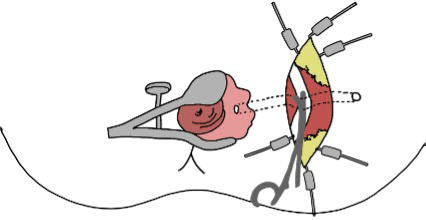
In a rectal advancement flap surgery, your surgeons will mobilize your healthy rectal tissue and create a flap. This is then advanced and sutured over the internal opening of the fistula to promote healing. Once the internal opening heals, the rest of the fistula will heal as well, leading to closure of the external opening. Everything happens within the rectum and no external stitches or wounds will be apparent, which means that no wound care is required.
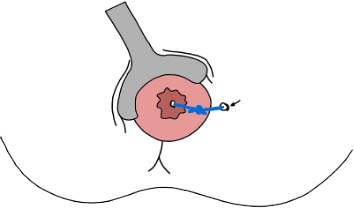
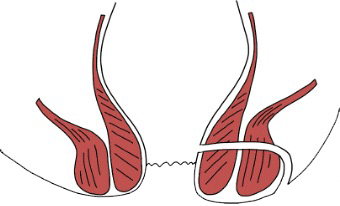
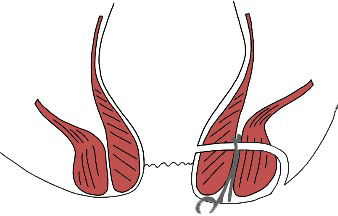
Ligation of the Intersphincteric Fistula Tract (LIFT) procedure
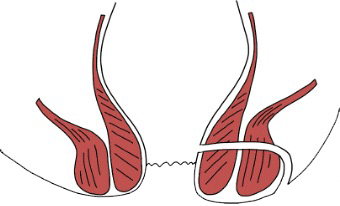
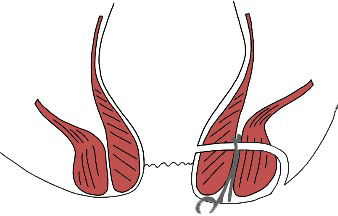
During a ligation of the intersphincteric fistula tract (LIFT) procedure, your surgeon will make a small incision close to the anus (between the anus and the external opening of your fistula) to find the fistula tract in between the sphincter muscles around the anus. To avoid cutting through the 2 circular sphincter muscles around the anus, the plane between both muslces is used to find the fistula tract. Once the fistula is found and isolated in the plane, it is ligated with sutures (closure of the internal opening). The incision made by the surgeon is then closed with stitches and may require some wound care.
Any surgical repair of a fistula in patients with Crohn’s disease is associated to a relatively high failure rate, resulting in a recurrent fistula. Please ask your surgeon to talk about the risk of recurrence which each technique.
Benign Perianal Diseases
A seton is a small, looped rubber band. Placement of seton drains is a common surgical intervention for managing perianal Crohn’s disease and benign perianal diseases, aimed at keeping the fistula open and to avoid recurrent peri-anal abscesses. Your surgeon will discuss with you when the seton can be removed.

In a rectal advancement flap surgery, your surgeons will mobilize your healthy rectal tissue and create a flap. This is then advanced and sutured over the internal opening of the fistula to promote healing. Once the internal opening heals, the rest of the fistula will heal as well, leading to closure of the external opening. Everything happens within the rectum and no external stitches or wounds will be apparent, which means that no wound care is required.
Any surgical repair of a fistula in patients with Crohn’s disease is associated to a relatively high failure rate, resulting in a recurrent fistula. Please ask your surgeon to talk about the risk of recurrence which each technique.
During a ligation of the intersphincteric fistula tract (LIFT) procedure, your surgeon will make a small incision close to the anus (between the anus and the external opening of your fistula) to find the fistula tract in between the sphincter muscles around the anus. To avoid cutting through the 2 circular sphincter muscles around the anus, the plane between both muslces is used to find the fistula tract. Once the fistula is found and isolated in the plane, it is ligated with sutures (closure of the internal opening). The incision made by the surgeon is then closed with stitches and may require some wound care.
Any surgical repair of a fistula in patients with Crohn’s disease is associated to a relatively high failure rate, resulting in a recurrent fistula. Please ask your surgeon to talk about the risk of recurrence which each technique.

